lv compliance | reduced left ventricular compliance
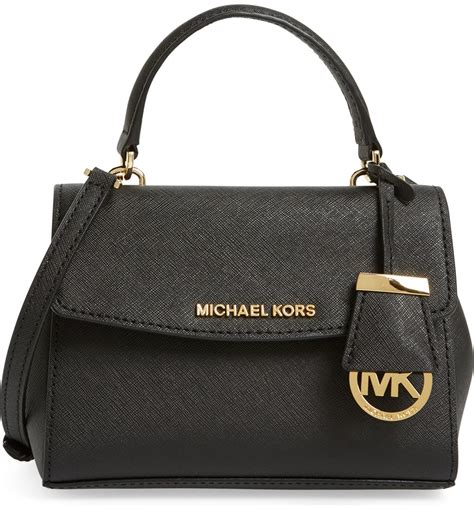
$255.00
In stock
Left ventricular (LV) compliance, often referred to as LV diastolic compliance, is a crucial determinant of cardiac function and overall cardiovascular health. It describes the ability of the left ventricle to expand and accommodate blood during diastole (the relaxation phase of the heart cycle) without a significant increase in pressure. In essence, it's a measure of the ventricle's stiffness or distensibility. A compliant ventricle readily accepts blood, allowing for efficient filling and optimal stroke volume. Conversely, reduced LV compliance, also known as increased LV stiffness, hinders diastolic filling, elevates ventricular pressures, and can lead to a cascade of adverse cardiovascular consequences.
This article delves into the intricacies of LV compliance, exploring the multiple factors that influence it, discussing the clinical implications of reduced or decreased LV compliance, and addressing frequently asked questions about this vital aspect of cardiac physiology.
Understanding Left Ventricular Compliance
LV compliance isn't a fixed property of the heart; it's a dynamic characteristic influenced by a complex interplay of structural, functional, and physiological variables. Mathematically, compliance (C) is defined as the change in volume (ΔV) divided by the change in pressure (ΔP):
C = ΔV / ΔP
A higher compliance value indicates a greater volume change for a given pressure change, signifying a more distensible and easily filled ventricle. A lower compliance value, on the other hand, reflects a stiffer ventricle that requires a greater pressure increase to achieve the same volume change.
Multiple Factors Affecting Ventricular Compliance
Several factors contribute to the complex regulation of LV compliance. These can be broadly categorized into intrinsic properties of the myocardium and extrinsic factors affecting ventricular loading and function.
* Age: Aging is a significant determinant of LV compliance. With increasing age, the myocardium undergoes structural changes, including:
* Increased Collagen Deposition: Collagen, a fibrous protein, provides structural support to the heart. However, with age, there's an increase in collagen deposition within the myocardium, particularly type I collagen, which is stiffer than type III collagen. This increased collagen content contributes to myocardial fibrosis, reducing ventricular distensibility.
* Myocyte Hypertrophy: Myocardial cells (cardiomyocytes) may enlarge with age, contributing to increased wall thickness. While initially compensatory, this hypertrophy can eventually lead to stiffening of the ventricle and impaired relaxation.
* Glycation of Collagen: Advanced glycation end products (AGEs) form when sugars bind to proteins, including collagen. Glycation stiffens collagen fibers, further reducing ventricular compliance.
These age-related changes collectively contribute to a decline in LV compliance, increasing the risk of diastolic dysfunction and heart failure with preserved ejection fraction (HFpEF) in older individuals.lv compliance
* Afterload: Afterload refers to the resistance against which the left ventricle must pump to eject blood into the aorta. Elevated afterload, such as that seen in hypertension or aortic stenosis, can acutely reduce LV compliance. Increased afterload leads to:
* Increased Ventricular Wall Stress: Higher afterload increases the tension within the ventricular wall, hindering relaxation and reducing the ventricle's ability to expand during diastole.
* Prolonged Isovolumic Relaxation: The isovolumic relaxation phase, the period between aortic valve closure and mitral valve opening, is prolonged with increased afterload. This delay in relaxation impairs early diastolic filling and reduces compliance.
Chronic elevation of afterload can lead to compensatory left ventricular hypertrophy, which, as mentioned earlier, can further decrease LV compliance over time.
* Myocardial Synchronization: Coordinated contraction and relaxation of the left ventricular walls are crucial for optimal diastolic filling and compliance. Asynchronous or dyssynchronous ventricular contraction, as seen in conditions like left bundle branch block (LBBB), disrupts this coordinated process, leading to:
* Prolonged Contraction of Some Segments: In dyssynchrony, some segments of the ventricle continue to contract while others are relaxing. This uneven contraction pattern impairs diastolic filling and reduces compliance.
* Increased Ventricular Wall Stress: Dyssynchrony increases wall stress in certain ventricular regions, further hindering relaxation and compliance.
Cardiac resynchronization therapy (CRT) aims to restore coordinated ventricular contraction in patients with heart failure and LBBB, thereby improving LV compliance and cardiac function.
* Intracellular Calcium Handling: Intracellular calcium (Ca2+) plays a critical role in both myocardial contraction and relaxation. Proper calcium handling is essential for normal LV compliance. Dysfunction in calcium handling can lead to:
* Impaired Calcium Reuptake: During diastole, calcium must be rapidly removed from the cytoplasm of cardiomyocytes to allow for relaxation. Impaired calcium reuptake by the sarcoplasmic reticulum (SR), the intracellular calcium store, prolongs myocyte contraction and reduces ventricular compliance.
* Increased Diastolic Calcium Levels: Elevated diastolic calcium levels can lead to incomplete relaxation and increased myocardial stiffness.
Conditions like heart failure and ischemia can impair calcium handling, contributing to reduced LV compliance.
* Myocardial Ischemia and Infarction: Ischemia (reduced blood flow) and infarction (tissue death) disrupt myocardial function and can significantly impair LV compliance.
Additional information
| Dimensions | 6.9 × 2.1 × 3.5 in |
|---|