lv contractility | left ventricle contractile
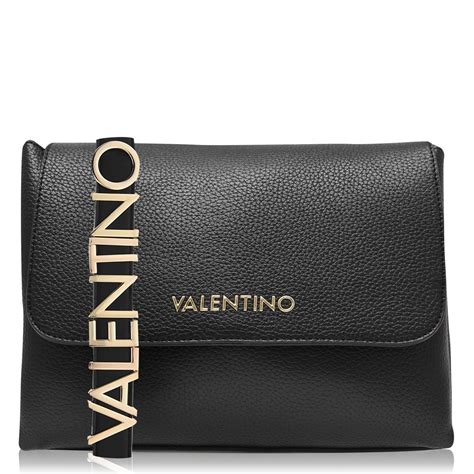
$298.00
In stock
Left ventricular (LV) contractility, also known as inotropy, refers to the intrinsic ability of the heart muscle (myocardium) to generate force and shorten, independent of preload and afterload. It’s a fundamental determinant of cardiac output and overall cardiovascular function. Understanding LV contractility is crucial in diagnosing and managing a wide range of cardiovascular diseases, from heart failure to valvular disorders. This article delves into the intricacies of LV contractility, exploring its measurement, regulation, and clinical significance.
Understanding Left Ventricular Contractility
The heart's primary function is to pump blood to meet the body's metabolic demands. This pumping action relies on the coordinated contraction and relaxation of the heart muscle. LV contractility represents the inherent strength of this contraction. It is determined by the number of active cross-bridges formed between actin and myosin filaments within the cardiac myocytes (heart muscle cells). A higher number of cross-bridges translates to a stronger contraction and a greater ability to eject blood from the left ventricle.
It's important to differentiate contractility from other factors influencing LV performance. Preload, afterload, and heart rate are all crucial, but they are *not* determinants of the intrinsic contractility. Preload is the degree of stretch of the ventricular muscle fibers at the end of diastole (filling phase), often represented by the end-diastolic volume. Afterload is the resistance against which the ventricle must pump, often represented by the systemic vascular resistance. While preload and afterload influence the *extent* of ventricular shortening and ejection, contractility dictates the *force* generated for that ejection, independent of these loading conditions. Think of it this way: preload is like stretching a rubber band, afterload is the weight you're trying to lift with it, and contractility is the inherent strength of the rubber band itself.
The LV Pressure-Volume Plane: Visualizing Contractility
The effects of altering preload, afterload, and contractility on LV performance are readily described in the LV pressure-volume (PV) plane. This graphical representation provides a powerful tool for understanding ventricular function.
* X-axis (Volume): Represents the left ventricular volume, typically in milliliters (mL).
* Y-axis (Pressure): Represents the left ventricular pressure, typically in millimeters of mercury (mmHg).
A single cardiac cycle is depicted as a closed loop on the PV plane, with four distinct phases:
1. Mitral Valve Closure to Aortic Valve Opening (Isovolumetric Contraction): The ventricle contracts, increasing pressure rapidly, but the volume remains constant as both the mitral and aortic valves are closed. This segment is nearly vertical on the PV loop.
2. Aortic Valve Opening to Aortic Valve Closure (Ejection Phase): The aortic valve opens, and blood is ejected from the ventricle into the aorta. The pressure rises initially and then gradually declines as the ventricle empties. The loop moves downward and to the left.
3. Aortic Valve Closure to Mitral Valve Opening (Isovolumetric Relaxation): The ventricle relaxes, and pressure decreases rapidly, but the volume remains constant as both the aortic and mitral valves are closed. This segment is nearly vertical on the PV loop.
4. Mitral Valve Opening to Mitral Valve Closure (Filling Phase): The mitral valve opens, and blood flows from the left atrium into the ventricle, increasing the volume. The pressure rises slightly. The loop moves upward and to the right.
The slope of the *End-Systolic Pressure-Volume Relationship (ESPVR)* is a key index of LV contractility. The ESPVR is a line connecting the end-systolic points (the point of lowest volume and highest pressure during ejection) of PV loops generated at different preload conditions. A steeper ESPVR indicates greater contractility, meaning the ventricle can generate higher pressure at a given volume. Conversely, a flatter ESPVR indicates reduced contractility.lv contractility
* Preload Effects: Increasing preload shifts the PV loop to the right, increasing both end-diastolic volume and stroke volume (the amount of blood ejected with each beat). However, the ESPVR remains unchanged unless contractility changes.
* Afterload Effects: Increasing afterload shifts the PV loop upwards and slightly to the left. Stroke volume decreases, and end-systolic volume increases. Importantly, an acute increase in afterload results in a greater proportion of the contractile energy being utilized to overcome the increased resistance, meaning less energy is available for ejection, even if the *intrinsic* contractility remains the same. Again, the ESPVR remains unchanged unless contractility changes.
* Contractility Effects: Increasing contractility shifts the ESPVR upwards and to the left. This leads to a steeper ESPVR, increased stroke volume, and decreased end-systolic volume at any given preload and afterload. The entire PV loop shifts upwards and to the left.
The PV loop analysis allows clinicians to visually assess how changes in preload, afterload, and contractility affect LV performance. For example, in heart failure with reduced ejection fraction (HFrEF), the ESPVR is typically flattened and shifted to the right, reflecting impaired contractility.
Factors Affecting Left Ventricular Contractility
Additional information
| Dimensions | 6.2 × 1.7 × 3.1 in |
|---|